Latest
News
What are Therapeutic Diets: 15 Common Examples & Precautions

Commonly used in hospitals, nursing homes, and medical nutrition therapy (MNT), therapeutic diets play an essential role in clinical nutrition, supporting treatment plans to improve the patient’s overall well-being.
In this article, we’ll explain the definition of therapeutic diets, why they’re prescribed, and explore their main types, including texture-modified, nutrient-controlled, and condition-specific diets, along with how supplements can support these dietary needs.
What is a Therapeutic Diet?
A therapeutic diet is a customized meal plan designed to support a medical treatment plan. It should be prescribed by a physician and developed by a registered dietitian to address individual health needs, such as managing diabetes, kidney disease, or recovery after surgery.
For a therapeutic diet to be effective, it must be personalized, nutritionally balanced, and realistic for the patient to follow, taking into account their ability and willingness to maintain the recommended dietary changes.
Reasons to Have a Therapeutic Diet
A therapeutic diet may be used to control the intake of specific nutrients, either by increasing (e.g., protein for wound healing) or decreasing (e.g., sodium for hypertension) them, to meet a patient’s altered metabolic needs. This focused control helps improve or reduce symptoms related to the underlying condition.
In some cases, texture modifications are also made to help those having trouble with chewing or swallowing. We’ll introduce the common meal plans as examples later on to help you get a clearer idea of this.
Ultimately, these diets allow patients to maintain or restore proper nutritional balance, and most importantly, to prevent complications that can arise from improper or restrictive eating, ensuring the body has the energy it needs to heal.
Common Types of Therapeutic Diets
Therapeutic diets are generally categorized based on their purpose, such as texture modifications, nutrient content adjustments, restrictions for food intolerances or allergies, and diets designed for specific medical conditions, according to hospital regulations and U.S. dietary guidelines.
In this section, we’ll provide an overview of common therapeutic diet types, but note that they are just for reference. Always consult a registered dietitian or healthcare professional before starting a therapeutic diet plan.
Therapeutic Diet Examples with Modified Texture

Source: Freepik
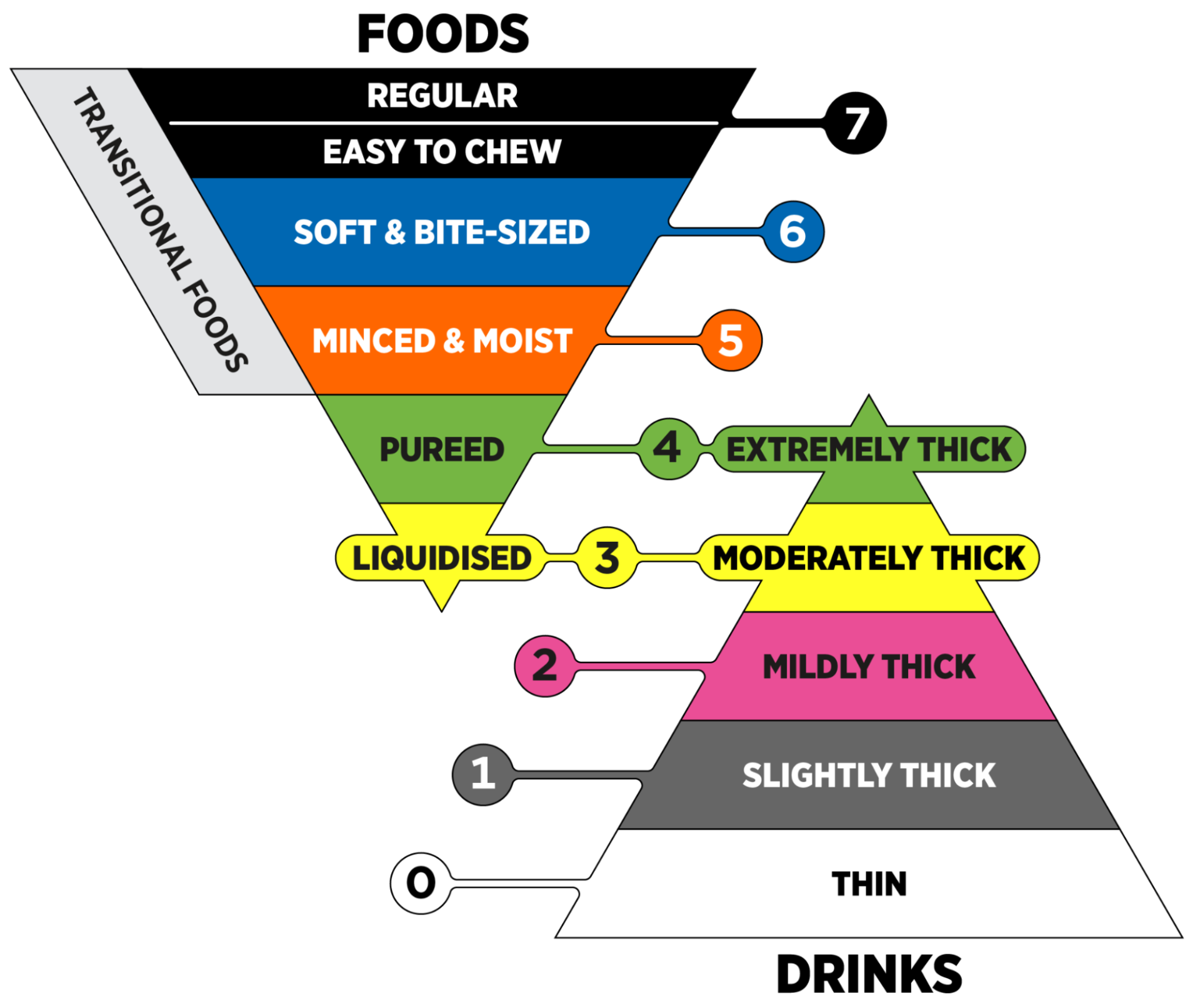
Texture-modified diets are vital for patients experiencing dysphagia (difficulty swallowing) or problems with chewing, often due to stroke, neurological disorders, or dental issues. These diets are standardized globally using the International Dysphagia Diet Standardization Initiative (IDDSI) framework, which uses 8 levels to describe food textures and drink thickness, as seen in the diagram below.
Source: The International Dysphagia Diet Standardisation Initiative
These therapeutic diet examples are all based on this framework:
Clear Liquid Diet
The clear liquid diet consists of thin, transparent fluids (at IDDSI Level 0) that are easily absorbed and leave minimal residue in the gastrointestinal tract. Examples include water, clear broth, apple juice without pulp, clear sodas, and gelatin without fruit pieces. Milk and other opaque beverages should be excluded since fat and casein usually leave residue.
It is typically prescribed before or after surgery, or for patients recovering from gastrointestinal disturbances like nausea or vomiting. Because this diet provides limited calories and nutrients, it should not be continued for more than a few days, as per the doctor’s or dietitian’s advice.
Full Liquid Diet
This diet includes all items from the clear liquid diet plus additional fluids and semi-liquids (usually at IDDSI Level 2) that are smooth at room temperature, such as milk, cream soups, custards, yogurt, and pudding. Foods with lumps, pulp, or particles should still be avoided.
It is often used as a transitional stage when patients can tolerate more than clear liquids but are not yet ready for solid foods. The full liquid diet provides more energy and protein but may still lack some essential nutrients if used long-term.
Pureed Diet
The pureed diet is designed for individuals with severe swallowing difficulties or those unable to chew, such as patients with advanced neurological conditions or those recovering from head or neck surgery.
Meals can include foods blended into a smooth, homogenous consistency that requires no chewing and can usually be eaten with a spoon (at IDDSI Level 4). Suitable options include pureed meats, mashed potatoes, thickened soups, and pureed fruits or vegetables. Each food is best prepared separately to maintain flavor variety. Still, avoid mixed-texture foods (e.g., soups with chunks) or items that may crumble, as they increase choking risk.
Soft Diet
The soft diet provides moist, tender foods that are easy to chew and swallow (at IDDSI Level 6). It is suitable for people with mild swallowing difficulties, dental issues, or recovering from oral or gastrointestinal surgery.
Food examples include finely chopped meats, soft-cooked vegetables, canned fruits, and tender grains. Just make sure that the foods have moisture and are cut into small, bite-sized pieces (typically no larger than 0.6 inches) to prevent choking. Raw vegetables, nuts, seeds, and tough meats should also be avoided.
|
Therapeutic Diet |
IDDSI Level |
Purpose/Who It's For |
Suitable Food Examples |
|
Clear Liquid Diet |
Level 0 |
Provides minimal residue. |
Water, clear broth, apple juice (no pulp), clear soda, plain gelatin. |
|
Full Liquid Diet |
Usually Level 2 |
A transitional stage when patients can tolerate more than clear liquids but are not ready for solids. |
All clear liquids, plus milk, smooth cream soups, custard, yogurt, and pudding. |
|
Pureed Diet |
Level 4 |
For individuals with severe swallowing difficulties or those unable to chew (e.g., advanced neurological conditions). |
Foods blended to a smooth, homogenous, pudding-like consistency (e.g., pureed meats and vegetables). |
|
Soft Diet |
Level 6 |
For individuals with mild swallowing/chewing difficulties or recovering from oral/GI surgery. |
Moist, tender foods cut into small, bite-sized pieces (e.g., finely chopped meats, soft-cooked vegetables). |
Therapeutic Diet Examples with Modified Nutrient Content
These diets are prescribed to manage medical conditions by adjusting the amount of specific macronutrients (carbohydrates, protein, fat) or micronutrients (sodium, potassium, etc.).

Source: Freepik
Low-Sodium Diet
A low-sodium diet limits salt intake to help manage fluid balance, blood pressure, and cardiovascular or kidney conditions. Typically, sodium intake is restricted to 2,300 mg (roughly 1 teaspoon of table salt) per day or less, though stricter limits may be recommended depending on the patient’s condition.
Foods to include in meals are fresh fruits and vegetables, unprocessed meats, plain grains, and low-sodium canned or frozen items. At the same time, foods high in sodium, such as bacon, cured meats, pickles, salted snacks, and canned soups, should be avoided. Always check food labels to track total sodium content, and never add table salt to meals. Consider seasoning them with herbs and spices instead.
No Added Salt (NAS) Diet
The NAS diet removes discretionary salt from meal preparation but allows naturally occurring sodium in ingredients. It is often used as a therapeutic meal for patients with hypertension, heart disease, or fluid retention while not requiring strict sodium restriction.
Suitable foods include fresh fruits, vegetables, unprocessed meats, and unsalted grains. As an alternative, meals may be seasoned with herbs, spices, or salt substitutes instead of table salt. Patients should also continue to avoid highly processed or pre-packaged foods high in hidden sodium and consult their dietitian for other safe seasoning alternatives.
Low-Fat / Low-Cholesterol Diet
Low-fat or low-cholesterol meals are used as therapeutic meals for managing cardiovascular disease, gallbladder disorders, liver disease, or pancreatic conditions. The diet typically limits total fat to 30% of daily calories and keeps cholesterol around 250-300 mg per day.
Recommended foods include lean meats, fish, low-fat dairy, fruits, vegetables, and whole grains, while foods high in saturated or trans fats, such as fried foods, fatty cuts of meat, and processed baked goods, should be minimized.
Nevertheless, patients should ensure intake of essential fatty acids from sources like fish, nuts, or plant oils within the allowed limits to maintain nutritional needs.
High-Fiber Diet
High-fiber diets, typically with up to 33 g or higher daily dietary fibre intake, aim to improve gastrointestinal function, adding stool bulk to promote normal bowel function for patients with constipation and non-inflammatory colon diseases like diverticulosis. They also support weight management, help control blood sugar, and manage cholesterol levels.
For this therapeutic meal, dietary fiber should come from a variety of sources, including fruits (like oranges, kiwis, and guavas), vegetables (like broccoli), whole grains, and legumes. Patients can increase the fiber in their meals gradually to prevent bloating or discomfort. Plus, sufficient fluid intake is crucial to help the fiber pass smoothly through the digestive system.
Low-Fiber / Low-Residue Diet
A low-fiber or low-residue meal may restrict daily fiber intake to less than 10-15 g. It is designed to reduce stool volume and irritation in the gastrointestinal tract, often recommended as a therapeutic diet for patients with diarrhea, inflammatory bowel disease (IBD), recent surgery, or acute flare-ups of gastrointestinal conditions.
Suitable foods include refined grains, tender cooked vegetables (like cucumber, pumpkin, zucchini without skins), canned or cooked fruits without skins or seeds (like melons, peaches, pears, etc), and lean meats. In the meantime, high-fiber foods such as raw vegetables, whole grains, nuts, and seeds should be avoided.
Since this diet can be restrictive, the patient might require supplements to receive enough vitamins and minerals.
High-Protein Diet
High-protein diets provide increased protein to support tissue repair, wound healing, immune function, or recovery from surgery or illness, especially for patients with malnutrition, chronic illnesses, or those undergoing intensive physical rehabilitation.
The protein intake may be increased to 15-20 calories per pound of body weight daily. Protein sources can include lean meats, poultry, fish, eggs, dairy products, legumes, and protein-enriched beverages. Doctors will have to monitor kidney function in patients with renal concerns and adjust protein intake accordingly under the guidance of a dietitian.
Controlled Protein Diet
Controlled protein diets regulate protein intake to reduce the buildup of nitrogenous waste in conditions such as chronic kidney disease, hepatic encephalopathy, or certain metabolic disorders.
Meals are mostly planned with more fruits, vegetables, and healthy fats. With most being less than 6 calories per pound of body weight daily, levels of protein intake restriction vary depending on the severity of the condition.
For example, patients with end-stage renal disease on dialysis may require moderate protein intake of 2.4 calories per pound of body weight with additional control of sodium, potassium, and phosphorus.
Controlled Carbohydrate / Diabetic Diet
Controlled carbohydrate diets, also known as diabetic diets, manage blood glucose levels through careful monitoring of carbohydrate intake, meal timing, and portion control. This diet is essential for patients with type 1 or type 2 diabetes, prediabetes, or gestational diabetes. It also supports weight management.
Suitable foods include whole grains, vegetables, fruits in measured portions, lean proteins, and limited amounts of low-fat dairy, based on the principles of the American Diabetes Association (ADA)’s Exchange List for Meal Planning.
Even while following the meal plans, patients should monitor their blood glucose regularly, coordinate meals with medications or insulin, and avoid foods with excessive added sugars.
No Concentrated Sweets (NCS) Diet
The NCS diet is a more flexible diet option compared to the controlled carbohydrate diet, sometimes used for diabetics whose blood sugar levels and weight are stable. It includes regular foods without added sugars, rather than strict calorie or carbohydrate counting.
Foods in this diet can include most regular meals with moderate amounts of fresh fruits, vegetables (especially non-starchy ones like cabbage and broccoli), whole grains, and lean proteins (like chicken, fish, tofu, beans, etc), but sources with added sugar should be limited, whether it’s desserts, cookies, cakes, candy, or sugar-sweetened beverages.
On top of that, patients should still monitor blood glucose levels and follow individual dietary recommendations from their healthcare provider.
|
Therapeutic Diet |
Purpose/Who It's For |
Suitable Food Examples |
Food to Avoid |
|
Low-Sodium Diet |
Manages hypertension, heart failure, and certain kidney conditions by limiting fluid retention. |
Fresh fruits and vegetables, unprocessed meats, plain grains, and low-sodium canned/frozen items. |
Bacon, cured meats, pickles, salted snacks, canned soups, table salt, and highly processed foods. |
|
No Added Salt (NAS) Diet |
A regular diet with no salt added during preparation, for patients needing a mild reduction in sodium. |
Fresh fruits, vegetables, unprocessed meats, and unsalted grains. |
Table salt packets, highly processed/pre-packaged foods with high hidden sodium. |
|
Low-Fat / Low-Cholesterol Diet |
Manages cardiovascular disease, gallbladder, liver, or pancreatic conditions by restricting total and saturated fats. |
Lean meats, fish, low-fat dairy, fruits, vegetables, and whole grains. |
Fried foods, fatty cuts of meat, processed baked goods, high-fat dairy, and trans fats. |
|
High-Fiber Diet |
Promotes normal bowel function for constipation and diverticulosis, while supporting metabolic health. |
Fruits, vegetables, whole grains, legumes, whole-grain breads, and cereals. |
No specific foods to avoid, but fiber intake should be increased gradually. |
|
Low-Fiber / Low-Residue Diet |
Reduces stool volume and intestinal irritation; for IBD flare-ups, diarrhea, or recent GI surgery. |
Refined grains, tender cooked vegetables, canned/cooked fruits without skins or seeds, lean meats. |
Raw vegetables, whole grains, nuts, seeds, tough meats, stringy vegetables. |
|
High-Protein Diet |
Supports tissue repair, wound healing, immune function, and recovery from surgery or malnutrition. |
Lean meats, poultry, fish, eggs, dairy products, legumes, protein-enriched beverages/supplements. |
No specific foods to avoid, but monitor for renal concerns and adjust intake as advised by a dietitian. |
|
Controlled Protein Diet |
Reduces the buildup of nitrogenous waste for chronic kidney disease and advanced liver disease. |
Increased fruits, vegetables, and healthy fats. Protein intake is tightly regulated based on severity. |
High-protein sources (meat, dairy) that would exceed the daily limit. |
|
Controlled Carbohydrate / Diabetic Diet |
Manages blood glucose levels, meal timing, and portion control; essential for diabetes and prediabetes. |
Whole grains, vegetables, fruits in measured portions, lean proteins, and low-fat dairy. |
Excessive added sugars, sugar-sweetened beverages, and uncontrolled portion sizes of carbohydrates. |
|
No Concentrated Sweets (NCS) Diet |
Eliminates foods with excessive added sugars for stable diabetics. |
Most regular foods, fresh fruits, vegetables, whole grains, and lean proteins. |
Desserts, cookies, cakes, candy, sugar-sweetened beverages, and foods with large amounts of added sugar. |
Therapeutic Diets Example for Food Intolerance/Allergy
These diets eliminate specific foods that trigger symptoms in the body. Though food intolerances usually cause discomfort and digestive issues, food allergies are particularly life-threatening as they involve an immune reaction. That’s why dietitians carefully plan these diets to ensure nutritional balance while avoiding the foods that are dangerous for the patients.

Source: Freepik
Gluten-Free Diet
A Gluten-Free Diet (GFD) is required for individuals with Celiac Disease, an autoimmune condition where gluten ingestion damages the small intestine lining, leading to nutrient malabsorption and severe symptoms. It is also necessary for those with a confirmed gluten allergy or non-celiac gluten sensitivity.
The diet involves the total elimination of gluten, a protein found in wheat, rye, and barley. While oats are naturally gluten-free, they are often excluded unless certified gluten-free due to the high risk of contamination during processing. On the other hand, suitable foods include rice, corn, potatoes, quinoa, certified gluten-free grains, fruits, vegetables, plain meats, and gluten-free dairy products.
In terms of food preparation, cross-contamination is a serious concern, particularly when eating out or using processed ingredients. That’s why patients should rely on dedicated equipment (e.g., counter-tops, toasters, cutting boards, etc.) and source ingredients very carefully to ensure the gluten content remains below the limit of 20 parts per million (ppm).
Lactose-Free Diet
A lactose-free diet is designed for individuals with lactose intolerance, a condition where the body cannot fully digest lactose, the sugar found in milk and dairy products. By avoiding or limiting the lactose sources, this diet reduces the risk of potential symptoms like bloating, gas, abdominal pain, diarrhea, or nausea.
Lactose-free options include lactose-free milk, hard cheeses, yogurt, and plant-based milk alternatives. Lactose-intolerant individuals may even choose to have small amounts of dairy combined with other foods to improve tolerance, or take lactase enzyme supplements to help digest lactose.
Bear in mind that lactose intolerance differs from a milk allergy, which requires complete avoidance of all dairy proteins. With this in mind, those avoiding dairy should make sure they get enough calcium and vitamin D, either through fortified foods or supplements.
Other Allergy-Modified Diets
Other allergy-modified diets involve the complete elimination of specific allergenic foods such as eggs, soy, peanuts, tree nuts, fish, shellfish, and certain additives. This is important for those with confirmed food allergies, which can provoke reactions ranging from mild discomfort to severe anaphylaxis, even with trace amounts of the allergen.
When eating or buying groceries, all ingredients should be carefully checked for hidden allergens. It is also important to avoid cross-contamination when preparing meals. Then again, appropriate substitutions should be made to maintain nutritional balance while avoiding the allergen.
|
Therapeutic Diet |
Purpose/Who It's For |
Suitable Food Examples |
Food to Avoid |
|
Gluten-Free Diet (GFD) |
Required for celiac disease, gluten allergy, and non-celiac gluten sensitivity. |
Rice, corn, potatoes, quinoa, certified gluten-free grains, fruits, vegetables, plain meats, and GF dairy. |
Wheat, rye, barley, and most oats (unless certified GF), malt, and products with potential gluten contamination. |
|
Lactose-Free Diet |
Manages lactose intolerance by avoiding or limiting lactose. |
Lactose-free milk, hard cheeses, yogurt with live cultures, and plant-based milk alternatives (e.g., soy, almond). |
Milk, soft cheeses, cream, butter, and products containing whey, casein, or lactose as an ingredient. |
|
Other Allergy-Modified Diets |
Complete elimination of specific allergens (e.g., peanut, egg, soy, fish) to prevent life-threatening immune reactions. |
Depends entirely on the specific allergy. |
All forms and derivatives of the specific allergen (e.g., eggs, soy, peanuts, tree nuts, fish, shellfish), including trace amounts. |
Therapeutic Diets Examples for Other Medical Conditions
Beyond the standard categories, certain medical conditions need highly specialized diets that fall into their own clinical niches. Common examples include the renal diet, autoimmune paleo (AIP) diet, and finger food diets. These plans often require continuous monitoring and the collaboration of an entire healthcare team for food safety, texture, and nutritional balance.
 Source: Freepik
Source: Freepik
Renal Diet
A renal diet is one of the most complex therapeutic plans, prescribed for patients with kidney disease, including those undergoing dialysis or with chronic kidney disease (CKD). Since damaged kidneys struggle to filter waste and balance electrolytes, this diet is highly individualized based on the patient's specific lab work and the stage of their disease.
With the primary aim of limiting the buildup of harmful substances, this meal often involves restricting sodium (to control blood pressure/fluid), potassium (to protect heart rhythm), phosphorus (to maintain bone health), and sometimes protein. Suitable foods often include fresh vegetables, low-potassium fruits (e.g., berries and apples), lean meats, rice, pasta, and specially formulated low-protein or low-sodium products.
As the restrictions on this diet need to constantly change according to lab results and dialysis, patients should work with a specialist renal dietitian during their treatment to manage their meal plans accordingly.
Autoimmune Paleo (AIP) Diet
The Autoimmune Paleo (AIP) diet is designed to manage autoimmune conditions, such as Hashimoto’s thyroiditis, rheumatoid arthritis, lupus, or inflammatory bowel disease. This diet emphasizes nutrient-dense, whole foods while removing common inflammatory triggers.
Allowed foods include meats, poultry, fish, vegetables, fruits, mushrooms, herbs, spices, and healthy fats. Foods to avoid include grains, dairy, legumes, nuts, seeds, processed sugar, and nightshade vegetables (e.g., tomatoes, peppers, eggplants).
Reminder, the AIP diet is a short-term, diagnostic tool and should not be used in a long-term lifestyle. After an initial healing period, foods must be slowly and systematically reintroduced to identify specific individual triggers. Moreover, this intense plan should only be followed under the guidance of a physician or dietitian to ensure patient safety.
Finger Food Diet
A finger food diet is designed for patients who have difficulty using cutlery due to conditions like stroke, dementia, Parkinson’s disease, arthritis, as well as other neurological or developmental disorders, which can impair cognitive function or mobility. It allows vulnerable patients to eat independently and at their own pace, improving their nutritional intake and quality of life.
Suitable options include bite-sized or easily held foods such as cut-up fruit, small sandwiches, chicken goujons, fish fingers, mini quiches, boiled eggs, vegetable sticks, and soft desserts.
Even though the food is meant to be eaten by hand, it should still be prepared with appropriate texture, temperature, and portion size to prevent choking. The meals should also cover all food groups to provide balanced nutrition.
|
Therapeutic Diet |
Purpose/Who It's For |
Suitable Food Examples |
Food to Avoid |
|
Renal Diet |
Manages Chronic Kidney Disease (CKD) and patients on dialysis by controlling sodium, potassium, and phosphorus intake for fluid and electrolyte balance. |
Low-potassium fruits, rice, pasta, fresh vegetables, lean meats, and specially formulated low-protein products. |
Foods high in potassium (e.g., bananas, tomatoes), phosphorus (e.g., nuts, dairy, whole grains), sodium (processed foods), and sometimes even protein. |
|
Autoimmune Paleo (AIP) Diet |
A short-term elimination diet to manage symptoms of autoimmune conditions (e.g., IBD, Lupus, Hashimoto's) by reducing inflammation. |
Quality meats, fish, most vegetables and fruits, herbs, spices, and healthy fats. |
Grains, legumes, dairy, nuts, seeds, eggs, processed sugar, and nightshade vegetables. |
|
Finger Food Diet |
Designed for patients with cognitive or physical impairments (e.g., dementia, stroke, arthritis) to promote independent eating. |
Foods cut into easily grasped, bite-sized portions: chicken goujons, mini sandwiches, soft fruit chunks, vegetable sticks, mini quiches. |
Foods that require utensils, have mixed textures, hard/tough meats, and are a choking hazard. |
Challenges and Considerations of Therapeutic Diets
Implementing a therapeutic diet may be helpful for treatment plans, but it also comes with challenges that could affect nutritional balance and overall quality of life:
-
Commitment and Adherence Issues: Therapeutic diets can feel too restrictive, especially when patients require multiple dietary modifications at the same time. Try gradual implementation, flexible meal planning, and providing appealing alternatives to help patients stick to the diet.
-
History or Risk of Eating Disorders: Prescribing restrictive diets to vulnerable patients can trigger disordered eating patterns, especially when they have a past eating disorder. In these cases, treatment must be handled with extreme caution and in collaboration with mental health professionals, sometimes prioritizing nutritional adequacy and positive food relationships over strict restriction.
-
Decrease in Quality of Life: Sometimes the diet may create more distress than the symptoms it relieves due to prep time, cost, and limited social eating. Dietitians can help by incorporating patient preferences and occasional safe indulgences while maintaining the restrictions necessary for medical stability.
-
Nutrient Gaps: Eliminating certain foods may lead to deficiencies. It is also important to work closely with a certified dietitian to avoid this, as they can help with careful meal planning and selecting fortified foods/supplements to fill these gaps.
-
Food Diversity: Limited options can cause boredom and reduce dietary variety. Rotating between foods and introducing new textures/flavors can improve satisfaction, allowing patients to continue enjoying meals.
Dietitians and healthcare providers will continuously monitor patients, adjusting or liberalizing diet orders as needed to ensure nutritional adequacy and maintain a positive relationship with food. Patients should always follow their advice and ask questions if problems arise.
The Role of Supplements in Therapeutic Diets
Supplements can support therapeutic diet nutrition, particularly for patients following restrictive or specialized eating plans. They can help fill nutritional gaps that may arise when certain foods are limited or eliminated, ensuring patients receive adequate vitamins, minerals, protein, and calories.
Furthermore, supplements like fortified meal replacements provide an additional option, introducing variety into the diet, offering flavors, textures, or nutrient combinations to prevent food boredom.
Supplements can also add flexibility, as they can be consumed with meals or between meals, depending on individual needs and schedules, even when appetite is low or meal preparation is challenging.
Nonetheless, patients still need to consult with their healthcare provider or dietitian before starting any supplement. This ensures the supplement is safe for their condition and aligns with their treatment plan.
Grace Biotech: Supplement Development to Support Therapeutic Diets
As a trusted manufacturer, Grace Biotech specializes in developing high-quality nutritional supplements that support therapeutic diets for patients with specific medical needs. By working closely with healthcare providers and brands, we offer customized solutions that ensure patients receive essential nutrients while adhering to dietary restrictions.
Our expertise spans formulation, ingredient sourcing, and dosage optimization, allowing for tailored ready-to-drink products that address nutritional gaps while maintaining treatment outcomes and quality of life. The products we’ve created include:
|
|
Diabetes Formula Designed for those managing blood sugar, this supplement provides low-glycemic carbohydrates, high biological value proteins, along with essential vitamins and minerals to support stable glucose levels and overall health.
|
|
|
Kidney Disease Formula (Non-Dialysis) Tailored for patients with impaired kidney function, this formula offers reduced protein, phosphorus, and potassium while ensuring sufficient calories and nutrients to prevent malnutrition risks.
|
|
|
Dialysis Formula This supplement supports patients on dialysis by replenishing lost protein, controlling mineral intake, and providing high-calorie nutrition to maintain strength.
|
|
|
Cancer Formula High in protein, calories, and antioxidants, this formula helps cancer patients combat muscle wasting, weight loss, and nutritional deficiencies during treatment.
|
|
|
Twocal Formula This is a concentrated, high-calorie liquid supplement that supports recovery, weight gain, and lean body mass maintenance for patients with increased nutritional needs.
|
Learn more about our services today, and let Grace Biotech provide you with end-to-end support from formulation to production.
Resources:
[1] Types of Therapeutic Diets. California Department of Social Services.
[2] Therapeutic Diet Manual. New York State Department of Correction and Community Supervision.
[3] Therapeutic Diet Manual. Oklahoma Department of Corrections.
[4] Diet Manual for Long-Term Care Residents. Maryland Department of Health and Mental Hygiene.
[5] Therapeutic Diets: Adjusting Nutrients and Texture. Illinois State Board of Education.
[6] Therapeutic Diets. The Association of UK Dietitians.






